The word fistula defines anomalous communication between two body surfaces, in this case between the rectal mucosa and the skin around the anus.
INDEX:
1. WHAT IS ANAL FISTULA
2. WHAT ARE THE CAUSES
3. THE SYMBOLS OF THE ANAL FISTULA
4. FERTILIZER TREATMENT
5. GENERAL INFORMATION AFTER INTERVENTION FOR ANAL FISTULA
6. GENERAL INFORMATION AFTER INTERVENTION FOR ANALYTIC FISTOLOGY WITH "CLOSED" TECHNIQUES
1. WHAT IS ANAL FISTULA
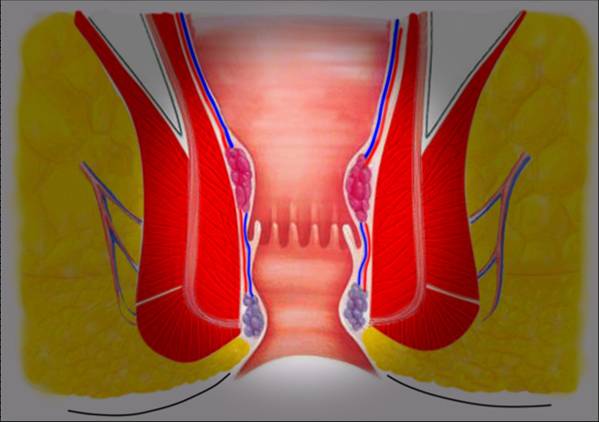
The word fistula defines anomalous communication between two body surfaces, in this case between the rectal mucosa and the skin around the anus.
2. WHAT ARE THE CAUSES
As with abscess, most of the fistulas are caused by infection of the glands within the anus, cryptomandular infections.
Depending on the site, the fistulas are divided into 4 types: Interspecific, Transfrequent, Superfractical and Extraspure.
3. THE SYMBOLS OF THE ANAL FISTULA
Often the fistulas are manifested as an abscess, but not always. Sometimes patients report the spillage of badly-blushed pus from a "forearm" around the anus.
Often they come from the doctor after years because the course can be alternated with long phases of complete but apparent healing. This attitude, however, is wrong, the more time it takes and the more chances are that other complications come to the fore, such as the formation of abscesses and other fistulas that make the intervention more complex.
The diagnosis is carried out with a proctological examination, possibly associated with ANOSCOPY and TRANSRATED ECOGRAPHY.
MAGNETIC RESISTANCE is useful in recurrences and in more complex cases. ALWAYS consider the need to perform a COLONSCOPY to exclude chronic intestinal inflammatory diseases and any other associated pathology of the rectum and the colon.
4. FERTILIZER TREATMENT
The principles for treating the fistula are three:
Eliminate the fistula, prevent recurrences, retain the function of the anal sphincter.
Surface fingers can be simply engraved throughout the journey while those passing through the sphincter can be treated with a "silk" ie passing a silk thread from the outer skin, fracture of the fist along the way to the inside of the rectum or Ano and causing it to escape from the anus. The silk is then knotted.
It's an extremely simple, sometimes out-patient procedure.
The setone is spontaneously eliminated from the body within a few months by slowly cutting off the sphincter, which simultaneously heals by healing, the risks are minimal and relapses are scarce.
The disadvantage is the presence for months of a silk thread.
Other conservative treatments are the removal of the fistulas through the sphincter muscle, the closure of the hole, the inside of the anus and the closure of the entire wound with suture points.
Healing is quick and after 15 days the points are removed (sometimes I do not put them on and I use a glue).
If the suture holds the healing is quick, but sometimes the infection causes the points to open and therefore the need to heal the wound by second intention, that is, with medication.
Two methods are more recent: the so-called Video Assisted Anal Fistula Treatment (VAAFT) consisting of entering the fistula hole with an optic, that is, a camera with a light source and an operating channel (the fistuloscope) that burns the fistula to its Entry into the rectum.
Then, with a suturing machine, the inner passage is closed hermetically.
The results are satisfactory and the technique invented by an Italian physician, Dr. Meinero, is spreading rapidly with encouraging results.
Another technique is to obey the fistulant by inserting material inside.
The use of cyanoacrylate, fibrin, and others has been attempted, but the best results were obtained with the use of small wrist prostheses (anal fistula plug) to be inserted inside the outer casing with careful attention To close the internal through the rectum. Technique too little invasive.
Compared to fistulectomy and silk the latter two techniques are more expensive for the material used.
5. AFTER OPERATION FOR ANAL FISTULA
After surgery, the anal area remains painless thanks to a painkillers treatment at fixed doses and times that will continue to be home and allow for regular life.
Probably at the level of the wound there is a gauze or surge that will be replaced during the ambulatory dressings that will be initially bi- or tri-weekly.
They are not painful dressings, gauze will be gently detached after they are wet.
Defecation is no longer a worrying event, if it does not happen spontaneously within 2 days, you will be given a mild laxative. It could be accompanied by red blood, mixed with clots and loss of "sapphire". No worries, just wash with plenty of water and betadine soap or eucloline: 2 sachets loose in the bidet water, using disposable gloves if necessary. We will think about the surgeon during the subsequent dressing to reposition it.
If it is present, the "silk" does not need any attention. Do not stay long on the water and do not use toilet paper. It may be useful to use the shower phone to remove any debris. Use a "donut" if necessary to avoid crushing the wound from sitting. Work can be taken between the 5th and 10th day after the intervention.
During the postoperative period, he or she may have a regular life avoiding long journeys for seven days, bicycle and motorbike for at least 2 weeks. It will have to boost a rich fiber supply and eliminate alcohol, coffee, chocolate, spices and spicy foods. We recommend for the first 7-10 days to apply an analgesic ointment before and after defecation.
After the intervention you can observe one of the following situations:
- Pain, anal and rectal burn, especially if you do not follow the analgesic therapy at a time.
- Loss of red or pink, then yellowish, slightly mild, even deodorant blood, which lasts until the last incision (1-3 months) is completely cleaved. Frequent washing with water is advisable. It is useful to use absorbents.
- Irritation of the skin around the anus which appears reddened and it causes itching and burning. It is caused by leaks or the use of gauze and absorbent or local ointments. These are protective creams.
- Temporary difficulty in holding gas. It is caused by dilation of the anus muscle fibers and disappears in about 1 week.
- Fever (up to 38 ° C) in the first days after surgery.
These situations are normal and planned and should not be a concern, otherwise they will have to alert the surgical team promptly.
6. AFTER-INTERVENTION INSTRUCTIONS FOR ANALYTICAL FISTOLOGY WITH "CLOSED" TECHNIQUES
After surgery, the anal area remains painless thanks to a painkillers treatment at fixed doses and times that will continue to be home and allow for regular life.
Probably the wound is closed with a "glue" or there are suture points.
The first dressing will be performed from 5 to 7 days after surgery. Defecation is not a worrying event, if it does not occur within 2 days, you will be given a mild laxative.
It could be accompanied by live red blood, mixed with clots from the internal wound and the loss of a hemostatic sponge that fits into the anus during surgery and turns into a dark red gel.
No concern, wash with plenty of water and EUCLORINA:
2 loose bags in the bidet water using disposable gloves, or with dedicated soaps (ANONET).
Do not stay long on the water and do not use toilet paper.
It may be useful to use the shower phone to remove any debris.
It is important to avoid crushing the wound, for at least two weeks. Therefore, at this time, you can only sit on a "donut" that will avoid traumatizing the sore from sitting.
Work can also be taken only two weeks after the intervention.
During the postoperative period, the patient may have a regular life avoiding long journeys for 7 days, bicycle and motorbike for at least 2 weeks.
Power will be rich in fiber by eliminating alcohol, coffee, chocolate, spices and spicy foods. No anal ointments are required.
After surgery the patient can observe one of the following situations:
• Pain, anal and rectal burns, especially if it does not follow the prescribed therapy.
• Loss of red or pink blood, then yellowish, slightly mild
Frequent washing with water is advisable.
The use of absorbents is useful.
• Irritation of the skin around the vessel which appears reddened and it causes itching and burning. It is caused by leaks or the use of gauze and absorbent or local ointments. They are with protective creams (Es: TROFO 5).
• Temporary difficulty in holding gases. It is caused by dilation of the anus muscle fibers and disappears in about 1 week.
• Fever (up to 38 ° C) in the first days after surgery.
For any further information or, if necessary, we are available at our contact details, provided that during the first three days of the intervention you will have to phone between 19.00 and 20.00 to one of your surgeons in your operating team to report on their status ( Possibly leave a message in the answering machine).


.JPG)